 The tools currently available to prevent, diagnose and treat TB are simply not up to the job. They were developed in an age before the HIV epidemic caused a huge upsurge in TB, and don’t meet the treatment challenges posed by issues such as stigma and poverty.
The tools currently available to prevent, diagnose and treat TB are simply not up to the job. They were developed in an age before the HIV epidemic caused a huge upsurge in TB, and don’t meet the treatment challenges posed by issues such as stigma and poverty.
The BCG vaccine is the most widely used vaccine in the world; yet 9 million people develop TB each year. TB is curable; yet 1.5 million people die from the disease each year.
Vaccination
The BCG vaccine is over 100 years old. At best, the BCG is 80% effective in preventing tuberculosis for a period of 15 years – but it doesn’t work for everyone. The BCG is:
- most effective in preventing severe forms of TB in children, such as TB meningitis
- of limited effectiveness against pulmonary TB in adults – the only form of infectious TB
- of limited effectiveness when given to people over the age of 35
- associated with disseminated BCG disease in HIV-infected infants
- less effective when given in equatorial regions.
New vaccines are crucial to eliminating TB, but they need to be effective for all age groups, for all forms of TB, and safe for people infected with HIV.
Diagnostics
Microscopy is the most widely used diagnostic test for TB. It is relatively cheap and does not require specialist facilities. Microscopy is effective in identifying active, pulmonary TB in adults – the most common form of TB and the only form of the illness that is potentially infectious. However, the test cannot identify drug-resistance and it is not sensitive enough to identify TB in children, people living with HIV and people with extra-pulmonary TB — because they have fewer bacteria in their sputum. This can delay diagnosis, which has implications both for the patient’s health and for controlling the spread of TB, including drug-resistant forms.
Culture tests, on the other hand, do provide a definitive diagnosis and identify drug-resistance. However, they are slow, expensive and require laboratory facilities and specialist staff, which are not available in many places.
The TB world desperately needs a single diagnostic test that:
- is affordable and suitable for use throughout the developing world, where specialist staff and laboratories – and even a regular supply of electricity – may not be widely available
- gives immediate results, as people are frequently lost to TB services before they can receive a diagnosis and treatment, often because they cannot afford the costs of return travel
- is sensitive and specific: to identify whether TB is active or latent, and the risks that latent TB will go on to become active; to identify drug-resistant TB; to identify TB-HIV co-infection; and to identify TB in children.



Drugs
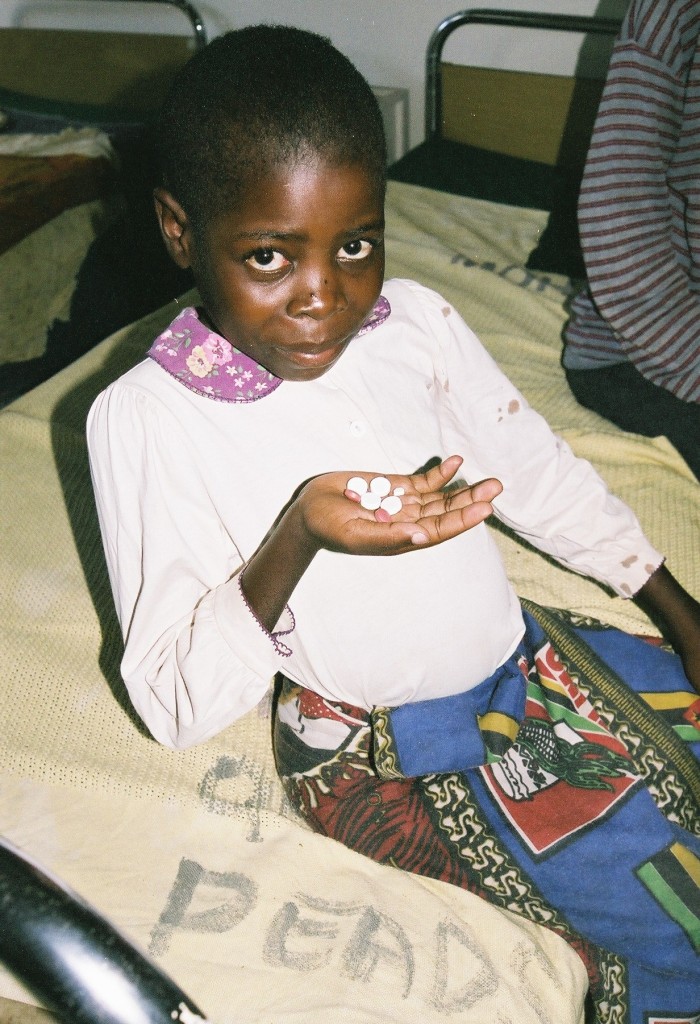
The current treatment regimen for drug-sensitive TB is effective in over 90% of cases. However, the treatment process is long and arduous – particularly so for children, as there are no paediatric formulations available. Treatment takes at least six months and many patients report unpleasant side effects. Patients often miss doses, or fail to complete their course of medication as a consequence. This can result in the return of symptoms and drug-resistance.
Treatment of multi-drug resistant TB (MDR-TB) is costlier and more challenging. The drugs are less effective, more toxic, and treatment regimens are longer. At best, MDR-TB can be cured in just 70% of patients.
Current TB medications were introduced between the 1950s and 1980s, in the early years of the global HIV epidemic, and before the link between TB and HIV was widely recognised. Since that time, there have been great advances in treatment for HIV with the advent of anti-retroviral therapy (ART). Advances in treatment for TB have not kept pace.
Research and development
With a potential market of 9 million people annually, you might imagine that a huge amount of research and development time and money is channelled into TB. This is simply not the case. TB is concentrated among the poorest people in the poorest countries of the world, so there is little market incentive to address the illness.
Until 1993, when the World Health Organization declared TB a global health emergency, there was also very little political incentive for research and development into TB. Things have slowly begun to change. In 1998, the Global Stop TB Partnership was launched, providing a combined force for the TB world to identify areas of need and drive through change, and developing a roadmap of research goals for TB.
