TB has been with us for thousands of years. Evidence of tuberculosis has been found in Egyptian mummies thousands of years old, and TB was thought to be common both in ancient Greece and Imperial Rome.
The 19th century
Deaths from TB peaked in the 1800s, as people crowded together in appalling urban environments when the industrial revolution steamed forwards. Infamously, TB caused the deaths of many notable poets, artists and composers of the time: DH Lawrence, Emily Brontë, Frédéric Chopin and Robert Louis Stevenson, to name but a few.
In 1854, Hermann Brehmer introduced the concept of fresh air, good nutrition and isolation in sanatoria, in an attempt to cure TB for the first time. This model was based on his own experience of successfully recovering from TB, after spending time in the clear air of the Himalayas. Treatment in sanatoria, and a gradual improvement of living conditions, started a slow decrease in TB cases in the 1900s. This fall in cases accelerated dramatically as innovations in diagnosis and treatment were born out of this new, scientific age.

In 1882, Robert Koch discovered M. Tuberculosis; in 1895, Wilhelm Konrad Röntgen discovered X-rays; and in 1908 Albert Calmette and Camille Guérin built on Louis Pasteur’s principle of vaccination to develop the Bacille Calmette-Guérin vaccine against tuberculosis.
New treatments
In 1944, Schatz, Bugie, and Waksman reported their discovery of the first medication shown to be effective against Mycobacteria tuberculosis, Streptomycin. This was a huge step forward, although the benefits of Streptomycin were limited by its toxicity and the ability of TB bacteria to develop resistance. Then, two years later, para-aminosalicylic acid (PAS) – a new medication developed by Jörgen Lehmann, began to be used alongside Streptomycin. Again, the benefits of PAS were short lived, as Mycobacterial resistance developed to this medication as well.
In 1951, scientists at Germany’s Bayer Chemical, and two US pharmaceutical companies, Squibb and Hoffmann-La Roche, all discovered Isoniazid – at the same time. Isoniazid proved to be powerful, safe, and inexpensive.
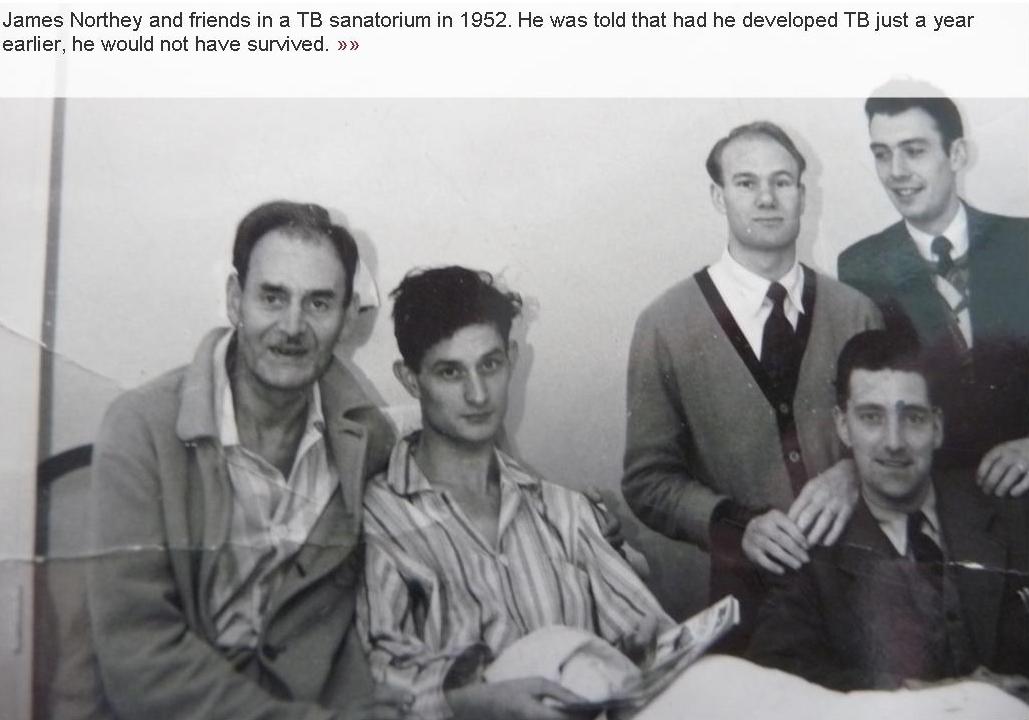
Following this, Sir John Crofton, a TB expert at the University of Edinburgh and founder of TB Alert, proposed that a combination of these three medications could completely cure TB if used from the outset of an individual case. This radical approach, which halved TB notifications in Edinburgh over a three-year period, was initially met with disbelief, but Sir John’s findings were soon replicated in a large scale international trial. As a result of combined therapy, sanatoria closed and earlier interventions to attempt to treat TB, such as thoracoplasty, became obsolete.
In the mid-1960s, modern ‘short-course therapy’ was introduced, using the newly available Rifampicin and the reintroduced Pyrazinamide – an old, toxic medication that was given a new ability to treat TB under the combined therapy model. This remains global gold standard treatment today. Although this treatment is effective, there are more people infected with Mycobacterium tuberculosis in the world than ever before.
A slow decline
The opportunity to eradicate TB was simply never realised, in part due to the inherent limitations of current TB tools for prevention, diagnosis and treatment; the failure of national and international policy for TB control; and the arrival and spread of HIV.
Today, cases of TB are declining on a global scale, in part due to the enormous efforts made towards preventing the spread of HIV. Yet the rate of decline remains slow and TB remains one of the leading infectious disease killers around the world. Furthermore, the emergence of drug-resistant strains of TB now threatens a return to a time when we were unable to control TB.
The future
While rates of TB are expected to continue to drop, the WHO sets out five priority actions to accelerate progress against TB. These are to:
- reach the three million people who currently miss out on TB treatment every year, through improving health systems and raising awareness
- address MDR-TB as a public health crisis, improving the capacity of countries with high rates of MDR-TB to diagnose and treat the disease
- ensure TB-HIV co-infection is a priority – increase coverage of ART for HIV-positive patients towards 100% and expand TB preventive treatment among people living with HIV
- increase funding to ensure the resources are available globally to control TB
- ensure new tools and strategies for better diagnosis, treatment and prevention of TB can be implemented rapidly in countries around the world.
